CASE-3: Pseudo-hyperkalaemia
Dr. Hani Ajrina Zulkeflee1, Dr Wan Nur Aimi Wan Mohd Zamri2, Dr Siti Nadirah Ab Rahim3, Dr Wan Nor Fazila Hafizan Wan Nik4 and Dr Razan Hayati Zulkeflee5
1Faculty of Medicine and Health Sciences, Universiti Sains Islam Malaysia, Bandar Baru Nilai, 71800 Nilai, Negeri Sembilan, Malaysia.
2Pathology Department, Hospital Ampang, Jalan Mewah Utara, Pandan Mewah, 68000 Ampang,Selangor, Malaysia.
3Pathology Department, Hospital Selayang, Lebuhraya Selayang – Kepong, 69100 Batu Caves,Selangor, Malaysia.
4Pathology Unit, Faculty of Medicine and Defence Health, National Defence University of Malaysia, Kem Perdana Sungai Besi, 57000 Kuala Lumpur, Malaysia.
5Department of Chemical Pathology, School of Medical Sciences, Universiti Sains Malaysia, 16150 Kota Bharu, Kelantan, Malaysia. 6Department of Haematology, School of MedicalSciences, Universiti Sains Malaysia, 16150 Kota Bharu, Kelantan, Malaysia.
Corresponding Author: Dr. Hani Ajrina Zulkeflee
E-mail: haniajrina@usim.edu.my
APFCB News Volume 3, Issue 1
Questions
1. What possibilities could you offer to explain the potassium results?
2. How to investigate the results?
3. What further tests to confirm the patient’s diagnosis and what is the underlying mechanism related to hyperkalaemia?
4. What is the best advice to clinicians when dealing with hyperkalaemia in this case?
Discussion
Question 1
Serial potassium results showed hyperkalaemia, which is diagnosed when the potassium concentration is above 5.0 mmol/L. It is particularly concerning when the level rises above 6.5mmol/L due to its potential cardiotoxicity risks.1
The patient showed no symptoms of hyperkalaemia such as palpitation, chest pain and muscle weakness. Her electrocardiography results showed no tall and tented T wave, shortened QT interval, widened QRS complex or absent T wave. Thus, pseudo-hyperkalaemia is suspected.
Pseudo-hyperkalaemia refers to an erroneous hyperkalaemia and it poses a significant challenge in the accurate determination of potassium concentration.2 Upon receiving hyperkalaemic results, the attending physicians are warranted to decide promptly, and this may result in injudicious administration of potassium-lowering therapies.
The possible causes of pseudo-hyperkalaemia include:
- Haemolysis of red blood cells (e.g. difficult venepuncture, improper specimen handling)
- In vitro leakage from other blood cells (e.g. thrombocytosis, leucocytosis)
- Potassium contamination (e.g. EDTA tube sampling, sampling at the same side of intravenous fluid).1
Question 2
Timely identification of pseudo-hyperkalaemia is crucial to prevent the administration of inappropriate treatments. A combination of severely elevated potassium concentrations reaching levels incompatible with life and asymptomatic presentation raises the suspicion of pseudohyperkalaemia.2 This shall be confirmed with a repeat sampling. Alternatively, utilizing a direct ion-selective electrode method through a blood gas analyser for the measurement of whole blood potassium offers a swift method to identify true hyperkalaemia, as it bypasses the technical processing of a patient’s sample.3
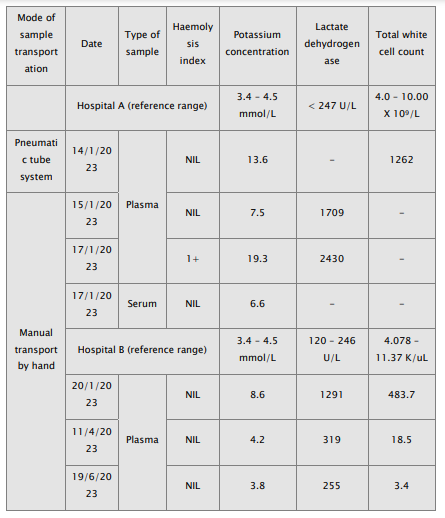
Red blood cell haemolysis is the predominant preanalytical factor leading to pseudohyperkalaemia. Any reported potassium concentration surpassing the reference range necessitates an accompanying assessment of the haemolysis index (H-index).4 Most of her results exhibited a negative haemolysis index, effectively ruling out haemolysis as the contributing factor
Reflex testing with serum calcium, magnesium, and alkaline phosphatase (ALP) helps mitigate the risk of K2-EDTA contamination. EDTA selectively chelates divalent cations, such as calcium and magnesium, leading to hypocalcaemia and hypomagnesaemia, respectively. Indirectly, depletion of these ions renders them inaccessible for various enzymatic reactions. For instance, ALP requires magnesium and zinc as the enzyme cofactors. Thus, this elucidates the observed low concentrations of ALP in samples contaminated with EDTA.5
Simultaneous measurement of serum and plasma potassium is beneficial for further investigation of its underlying cause. Reverse pseudo-hyperkalaemia refers to an elevated plasma potassium concentration compared to the serum levels observed in the presence of significant leucocytosis.6 Conversely, thrombocytosis leads to an increased measured serum potassium due to the release of potassium by platelets during the clotting process.7
Figure 1 depicts the proposed stepwise laboratory approach to hyperkalaemia, aiming for the early detection of erroneous results.

Figure 1: Diagnostic algorithm on approach to pseudohyperkalaemia
Question 3
Urgent blood film and bone marrow biopsy confirmed a diagnosis of Chronic Lymphocytic Leukaemia (CLL).
Dysplastic leukocytes in leukaemia are easily ruptured during sample centrifugation due to an increased in the membrane fragility. CLL for example, has cytoskeletal defects on its lymphocytes and this is manifested as smudge cells on peripheral blood film. In the presence of hyperleukocytosis, in vitro lysis of CLL lymphocytes can lead to the spurious hyperkalaemia. 2, 4
Serum potassium measurement yields a lower result as the fibrin clot in the serum captures and stabilizes delicate tumour cells during sample centrifugation, consequently minimizing therelease of potassium from the cells.7
The pneumatic tube system is not an appropriate method for sample transport in this case dueto the additional mechanical force exerted on the fragile leukemic cells. This is evident in the higher reported potassium concentration compared to the specimens transported manually byhand.
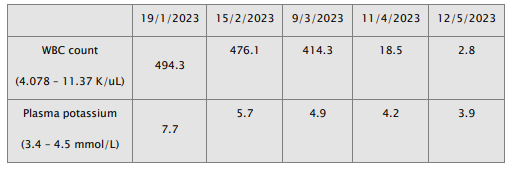
Chemotherapy was commenced, and serial laboratory results showed reduction of white bloodcell count along with plasma potassium levels. This showed that the magnitude of potassium elevation is proportional to the white cell counts as we can see the normalization of plasma potassium is achieved when the white cell counts reduced.
Question 4
This case highlights the importance of recognizing pseudo-hyperkalaemia in patients with extreme hyperleukocytosis. This awareness is essential to prevent iatrogenic hypokalaemia and ensure prudent patient management. The significance of identifying pseudohyperkalaemia isparticularly emphasized in this patient, as accurate electrolyte monitoring is crucial to assess the risk of tumour lysis syndrome during her chemotherapy treatment. 2,4
The most suitable method for monitoring the patient's potassium levels is through whole bloodpotassium analysis using a direct ion-selective electrode method through the blood gas analyser.3,8 This approach aids in distinguishing between true and erroneous hyperkalaemia Additionally, it is imperative for clinicians to correlate blood test results with clinical findings. Effective communication between clinicians and laboratory personnel becomes essential whenreported results show discrepancies.
1. Lindner G, Burdmann EA, Clase CM, Hemmelgarn BR, Herzog CA, Ma?yszko J, Nagahama M, et al. Acute hyperkalemia in the emergency department: a summaryfrom a Kidney Disease: Improving Global Outcomes conference. Eur J Emerg Med 2020; 27(5):329- 337.
2. Dewey J, Mastenbrook J, Bauler LD. Differentiating Pseudohyperkalemia From True Hyperkalemia in a Patient With Chronic Lymphocytic Leukemia and Diverticulitis. Cureus 2020 17;12(8):e9800.
3. Shrestha B, Rijal SS, Pokhrel A, Paudel A, Baral K, Poudel B, et al. Pseudohyperkalemia Associated With Leukemia. Cureus 2022; 14(4):e23978.
4. Haque MZ, Nasir A, Judge R. Pseudohyperkalemia in chronic lymphocytic leukemiaand diabetic ketoacidosis. Clin Case Rep. 2023 Aug 22;11(8):e7821.
5. Van Elslande J, Dominicus T, Toelen J, Frans G, Vermeersch P. A case of severe pseudohyperkalaemia due to muscle contraction. Biochem Med (Zagreb) 2020; 30(2):021004.
6. El Shamy O, Rein JL, Kattamanchi S, Uribarri J, Vassalotti JA. Reverse pseudohyperkalemia is more than leukocytosis: a retrospective study. Clin Kidney J2020; 14(5):1443-1449.
7. Merritt M, Kline H, Garimella S, Seigler R. Pseudohyperkalemia in a patient with T-cellacute lymphoblastic leukemia and hyperleukocytosis. J Pediatr Intensive Care 2018;7:166–168.
8. Massicotte-Azarniouch D, Canney M, Sood MM, Hundemer GL. Managing Hyperkalemia in the Modern Era: A Case-Based Approach. Kidney Int Rep 2023; 24;8(7):1290-1300.