Acute Pyelonephritis
Dr. Marilyn Masih1
1Senior Resident Department of Biochemistry G.B.Pant Institute of Postgraduate Medical Education & Research (GIPMER) Delhi, India
Corresponding Author: Dr. Marilyn Masih
E-mail: drmarilynmasih13@gmail.com
APFCB News Volume 2, Issue 2
On physical examination, the patient was found to be febrile with oral temperature 39.5°C, heart rate 93 bpm, and blood pressure 100/60 mm Hg. No signs of pallor, icterus or lymphadenopathy were seen. Chest and cardiac auscultation did not reveal any abnormality. On palpation, the abdomen was found to be soft and lax but there was right renal angle tenderness. The patient was admitted to medicine ward in view of persistent fever and recurrent urinary tract infections for further evaluation and laboratory investigations. The results as shown below (Table 1):
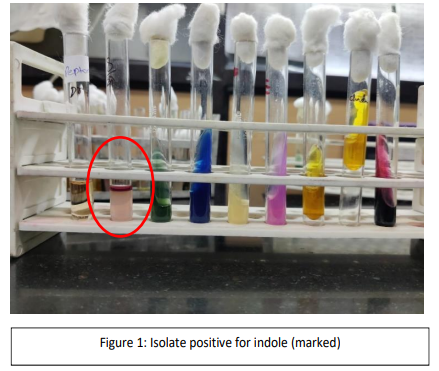
Laboratory Investigations
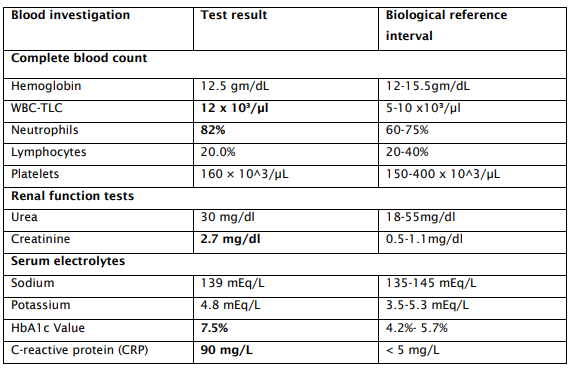
Routine investigations revealed high HbA1c value (7.5%) with normal serum sodium levels, normal levels of urea and haemoglobin. Serum creatinine was raised. TLC was also raised along with CRP depicting infection. Further blood culture test was ordered for which two sets of blood samples were collected in aerobic and anaerobic bottles; only one of the aerobic bottles was flagged positive in the after >48 hrs of incubation. The gram-stained smear of the sample from the positive blood culture bottle showed presence of gram-negative bacilli in clumps, and culture on blood agar plates also grew the same organism.
The isolate was positive for indole and catalase, whereas oxidase, citrate and urease were negative (Figure: 1).
Urine Examination
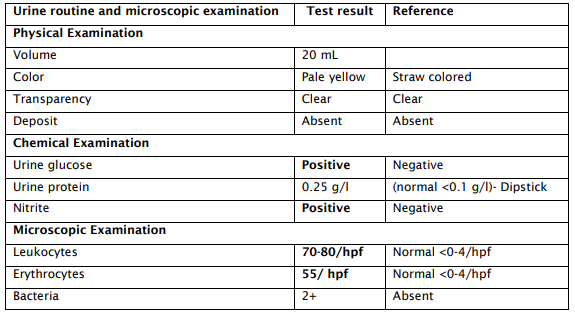
Urine Routine/Microscopy revealedurine protein 0.25 g/l (normal <0.1 g/l) by Dipstick, while glucose and nitrites were positive. Microscopy-revealed leukocytes 70-80/hpf (normal <0- 4/hpf), erythrocytes 55/hpf (normal <0–4/hpf) and bacteria 2+ (Table 2). Urine ketone bodies, bilirubin, urobilinogen, and leukocyte esterase were negative.
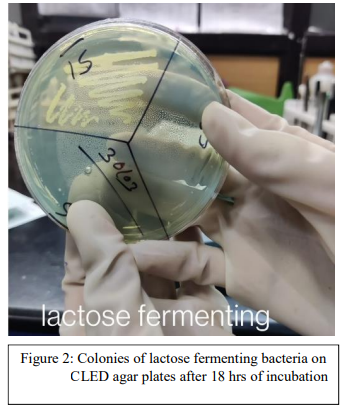
Urine sample was also collected for culture (clean catch mid-stream urine), which showed yield growth of E. coli on CLED agar plates after18 hrs of incubation (Figure: 2)
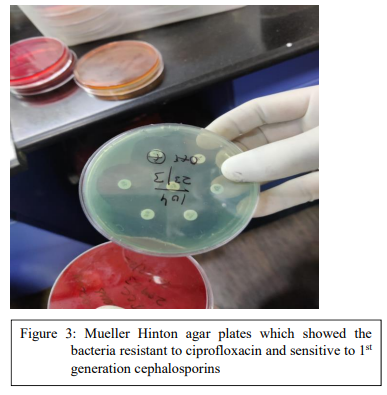
Antibiotic susceptibility testing (AST)
It was done by Kirby Bauer disk diffusion susceptibility test method on Mueller Hinton agar plates which showed the bacteria resistant to ciprofloxacin and sensitive to 1 st generation cephalosporin’s (Figure 3).
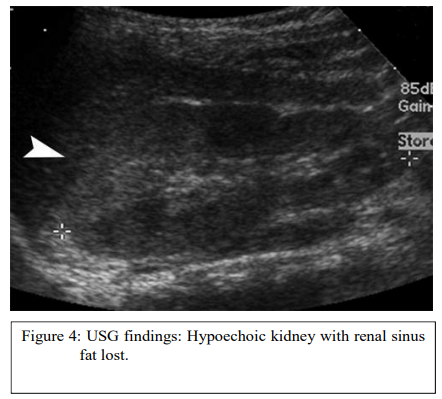
Radiological examination:
Ultrasound findings revealed enlargement of kidney in size with surrounding perinephric fat stranding along with ptheresence of calculi in the right kidney (Figure 4).
Interpretation & Analysis
Major hospital admissions due to lower urinary tract infections have a high chance of progressing to upper urinary tract and cause pyelonephritis. Inflammation of the renal parenchyma brought on by bacteriuria that travels from the bladder via the ureters and up to the kidneys is the hallmark of acute pyelonephritis.
In this case study, urinary analysis, radiological results, together with the recognized presenting symptom triad of nausea, fever, and flank pain allowed the practitioner to make the diagnosis of acute pyelonephritis. The diagnosis for Pyelonephritis was mainly done on the basis of clinical history, urine microscopy and culture and blood culture. Radiological findings of ultrasound helped rule out other possibilities such as a renal abscess and emphysematous kidney. Complications were ruled out by other biochemical blood investigations.
Being a female, known diabetic patient with history of recurrent episodes of UTI made the patient more prone to develop pyelonephritis. Urine culture which showed yield growth of E. coli on CLED agar plates, also led the way closer to the diagnosis, as E. coli is the most common bacteria to cause pyelonephritis. Furthermore, antibiotic sensitivity testing helped us know that the patient was resistant to ciprofloxacin treatment.
So correct line of treatment was started during her inpatient stay: IV ampicillin +1 aminoglycoside until afebrile till 24 hours, then oral antibiotics for 3 weeks. These antibiotics were adjusted accordingly after monitoring of AST results. Patient’s condition improved as reported in the follow up visits to the OPD.
Diagnosis:
ACUTE PYELONEPHRITI
1. Tietz Textbook of Clinical Chemistry and Molecular Diagnostics, seventh edition.
2. Song HK, Shin DH, Na JU, Han SK, Choi PC, Lee JH. Clinical investigation on acute pyelonephritis without pyuria: a retrospective observational study. J Yeungnam Med Sci. 2022; 39(1):39-45.
3. Hudson, C and Gerri Mortimore. The diagnosis and management of a patient with acute pyelonephritis. British journal of nursing. 2020; 29(3): 144-150.
4. Venkatesh L, Hanumegowda RK. Acute Pyelonephritis - Correlation of Clinical Parameter with Radiological Imaging Abnormalities. J Clin Diagn Res. 2017; 11(6):TC15-TC18. Georgi Abraham and others, Diagnosis of acute pyelonephritis with recent trends
5. Georgi Abraham and others, Diagnosis of acute pyelonephritis with recent trends in management, Nephrology Dialysis Transplantation. 2012; 27(9):3391–3394