Cardiovascular Disease Epidemic in India and Triglyceride-Associated Residual Atherosclerotic Cardiovascular Disease Risk
Pratishtha Mehra1, Vimal Mehta1, Jamal Yusuf1, Safal1, Pradeep Kumar Dabla2
1 Department of Cardiology, G. B. Pant Institute of Postgraduate Medical Education and Research, New Delhi, India
2 Department of Biochemistry, G. B. Pant Institute of Postgraduate Medical Education and Research, New Delhi, India
Corresponding Author:
Dr. Vimal Mehta, Director-Professor, Department of Cardiology G. B. Pant Institute of Postgraduate Medical Education and Research (GIPMER), New Delhi, INDIA
E-mail ID: drvimalmehta@yahoo.co.in
APFCB News Volume 3, Issue 1
EPIDEMIOLOGY
Cardiovascular (CV) disease is the leading cause of death in the world causing nearly one-third of all deaths. It has reached epidemic proportions in low- and middle-income countries with over three-quarters of total CV deaths occurring in these countries.1 India has one of the highest burdens of cardiovascular disease (CVD) with coronary heart disease prevalence rates in India ranging from 2% to 7% in rural populations and from 7% to 13% in urban populations.2,3CV disease was responsible for 26.6% of total deaths in India in 2017, compared with 15.2% in 1990. The Global Burden of Disease (GBD) study group reported a 2.3-fold increase in the prevalence of both ischemic heart disease (IHD) and stroke in the country between 1990 and 2016. Also, there was a two-fold increase in the number of prevalent cases of CV disease, from 25.7 million in 1990 to 54.5 million in 2016.4,5
Although the cardiovascular death rate in India is similar to Western populations, alarmingly Indians develop atherosclerotic cardiovascular disease (ASCVD) about a decade earlier than the Western populations, despite having lower levels of low-density lipoprotein cholesterol (LDLC).6 It has been reported that more than 50% of coronary artery disease (CAD)-associated deaths in India occur before the age of 50 years and 25% of myocardial infarctions (MI) occur before the age of 40 years.7In the INTERHEART study, the median age of MI among Indians was 53.0 years compared to 58.1 years in other countries.8
The high prevalence of CV disease can be attributed to the increased frequency of risk factors in the Indian population like sedentary lifestyle, unhealthy diet, obesity, metabolic syndrome, smoking, dyslipidemia, prediabetes, diabetes, and hypertension. Further, genetic predisposition, low-grade inflammation, and other known and unknown risk factors contribute to the increased prevalence.
According to International Diabetes Federation Atlas estimates, age-adjusted comparative prevalence of diabetes in India was 9.6% as of 2021.9 The prevalence of hypertension was 25.3% in the fourth District-Level Household Survey conducted in India from the year 2012-2014, with hypertension being common even among younger age groups (18-25 years).10 Dyslipidemia is also highly prevalent in India with the ICMR–INDIAB study reporting that 79% of Indian subjects have at least one lipid abnormality. The decreased high-density lipoprotein-cholesterol (HDLC) levels were found in 72.3% of subjects, hypertriglyceridemia in 29.5% and elevated LDL-C levels were identified in 11.8% of subjects.11
MANAGEMENT OF ATHEROSCLEROTIC CARDIOVASCULAR DISEASE RISK
The institution of lifestyle measures is key to decreasing the risk of ASCVD including avoiding smoking and alcohol, regular exercise, preventing obesity, heart a healthy diet, and optimal management of hypertension and diabetes. Since the incidence of diabetes is increasing and the incidence of prediabetes is 2-3 times that of diabetes, patients with prediabetes must be managed appropriately to circumvent the onset of diabetes and ultimately reduce the risk of developing ASCVD.
Low-density lipoprotein cholesterol (LDL-C) lowering to reduce CV risk
LDL-C has both a causal and a cumulative effect on the risk of atherosclerotic cardiovascular disease. In all the major guidelines across the globe for dyslipidemia management, LDL-C is the primary target for ASCVD risk reduction. The LDL-C goals have been a moving target with the recent American College of Cardiology (ACC) and European guidelines recommending LDLC goals of <55 mg/dL in very high-risk patients.12,13
The Lipid Association of India was the first organization in the world to recommend the LDL-C goal of <50 mg/dL in very high-risk patients in the year 2016 considering the increased risk of ASCVD in South Asian individuals. The statin therapy is the first-line therapy for management of dyslipidemia. The LDL-C levels are lowered by 30% with moderate-intensity statin therapy; high-intensity statins (HIS) reduce LDL-C by 50%. The combination therapy with HIS + ezetimibe reduces LDL-C levels by about 65%. The addition of bile acid sequestrants or bempedoic acid results in an additional LDL-C reduction of 20%.The proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors reduce LDL-C by about 55%-60%.14
Residual risk
Multiple randomized trials with statins have shown that statins reduce adverse CV events both in primary and secondary prevention. However, there is a huge residual risk despite the use of statins as approximately 75% of CV events cannot be prevented despite statin therapy.15Although newer non-statin therapies like ezetimibe, bempedoic acid, and PCSK9 inhibitors have been shown to reduce LDL-C levels beyond the 50-60% reduction seen with statins with additional CV benefit, still there remains a significant residual risk. Although part of this residual risk may be attributable to many conventional, non-conventional, and genetic risk factors as listed above, the lipid-associated risk is of extreme importance because it is the lipids that accumulate in the arterial wall to initiate atherogenesis. The lipidrelated risk is ascribed to several factors including non-attainment of LDL-C goals, hypertriglyceridemia, atherogenic dyslipidemia, small, dense LDL particles, remnant cholesterol (cholesterol in triglyceride-rich lipoproteins) and lipoprotein (a).
Triglycerides and cardiovascular disease
The triglycerides (TG) are transported in the blood by TG-rich lipoproteins. The TG-rich lipoproteins are chylomicrons (CMs) (?90% TG), very-low-density lipoproteins (VLDL) (?70% TG), intermediate-density lipoproteins (IDL) (?30% TG), chylomicron remnants and VLDL remnants (Figure 1). The remnants are derived from CMs secreted from the intestine and VLDL particles secreted from the liver as TGs are partially degraded by lipoprotein lipase (LPL) in the bloodstream. TGs are also present in small amounts (<10%) in low-density lipoprotein (LDL) and high-density lipoprotein (HDL) particles.
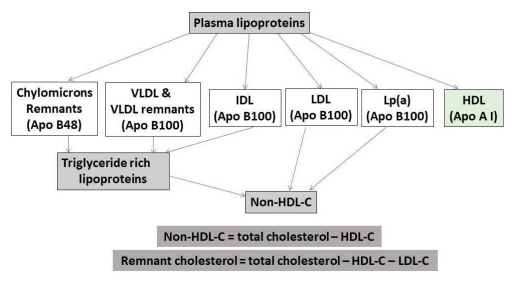
Figure 1. Triglyceride-rich apo B containing plasma lipoproteins
The normal plasma triglyceride levels are <150 mg/dL with optimal levels being ≤100 mg/dL, levels beyond 150 mg/dL are associated with ASCVD risk. This CV risk is typically present when triglycerides are moderately elevated (up to 500 mg/dL). The TG elevations ≥500 mg/dL are more of a concern about the risk of pancreatitis than ASCVD risk. The increased TG levels are often due to factors like increased fat intake, sedentary lifestyle, obesity, metabolic syndrome, insulin resistance, diabetes (especially uncontrolled), alcohol consumption, etc.; likewise, they also show a marked decrease in response to control of the above, making lifestyle interventions key to management of hypertriglyceridemia.16
Hypertriglyceridemia is a risk factor for atherosclerotic cardiovascular disease either directly or indirectly. It can be a manifestation of underlying atherogenic risk factors and diseases listed above or may be directly responsible as cholesterol in triglyceride-rich lipoproteins can get deposited in the arterial wall. As lipoprotein particles ≤70 nm in size can enter the arterial wall, VLDL, VLDL remnants, intermediate-density lipoproteins, and chylomicron remnants can infiltrate the arterial wall. Chylomicrons being very large and having a very short half-life are not atherogenic.
The triglyceride content of triglyceride-rich lipoproteins (TGLPs) gets hydrolyzed by the action of lipoprotein lipase, an enzyme present on the vascular endothelial surface to provide free fatty acids to peripheral tissues like muscle, adipose tissue, etc. for energy and storage. The cholesterol component of TGLPs is directly atherogenic. Moreover, the TG-rich lipoproteins can indirectly potentiate atherogenesis by potentiating inflammatory response by upregulating proinflammatory cytokine production and promoting thrombin generation. The pooled data from secondary prevention trials: the Cholesterol and Recurrent Events trial (CARE) and the Longterm Intervention with Pravastatin in Ischemic Disease study (LIPID) showed that TG levels remain a CV disease risk factor in patients treated with statins, with patients in the statin arms having increased event rates if TG levels were high.17 This suggests that control of both LDL-C and TGs may be important to achieve CV risk reduction. Since TG levels directly correlate with the remnant cholesterol (cholesterol content of TGLPs) levels, TG levels must be lowered therapeutically to reduce the CV risk.
Although statins lower TG levels by up to 35% based on baseline TG levels, certain drugs like fibrates, niacin, and omega-3 fatty acids decrease TG levels more significantly. However, earlier trials with fenofibrate, niacin, and a relatively low dose of omega-3 fatty acids (up to 1 gm/day) failed to show the significant benefit of these drugs in reducing the primary outcome in large randomized trials. However, in the REDUCE-IT (Reduction of Cardiovascular Events With Icosapent Ethyl- Intervention Trial) trial, 8179 high-risk patients (70% secondary prevention) with plasma triglyceride concentrations of 135-499 mg/dL were randomized to treatment with 4 g icosapent ethyl (a purified derivative of eicosapentaenoic acid (EPA)) daily or a mineral oil control and followed up for a median of 4.9 years. The high dose icosapent ethyl lowered the plasma triglyceride concentration by a median of 19.7% and reduced the risk of ASCVD events by 25% compared with the placebo, however, the reduction in ASCVD risk was unrelated to the change in plasma triglycerides.18In The EVAPORATE trial icosapent ethyl 4 gm daily demonstrated significant regression of low attenuation plaque volume on coronary computed tomographic angiography compared with placebo over 18 months. 19
Omega-3 carboxylic acid (omega 3 CA) formulation of omega-3 fatty acids (EPA and docosahexaenoic acid (DHA)) does not require hydrolysis by pancreatic lipase during intestinal absorption, eliminating the need for consumption with a high-fat meal, resulting in greater bioavailability compared with standard omega 3 ethyl ester formulations. The administration of 4 gm/day of omega 3 CA produces similar increases in plasma EPA levels as doses of purified EPA approved for clinical use, and also increases DHA concentrations. In the STRENGTH trial, 13,078 statin-treated patients with high CV risk, hypertriglyceridemia, and low HDL-C were randomized to omega-3 CA in a dose of 4 gm per day. The median baseline triglyceride level was 240 mg/dL and 70% of participants had diabetes. Triglyceride levels were reduced by 18% which was similar to REDUCE IT trial. CRP levels significantly decreased with omega-3 CA use vs. corn oil (–20% vs –6.3%; P <0.001). However, no significant difference in the composite outcome of major adverse CV events was seen.20
Although both REDUCE-IT and STRENGTH trials randomized subjects with hypertriglyceridemia with approximately the same baseline triglyceride levels, the STRENGTH trial did not show the benefit of omega-3 CA. STRENGTH trial used a combination of EPA and DHA, whereas the REDUCE-IT trial used only purified EPA.21
The EPA and DHA decrease the production of triglyceride-rich VLDL particles from the liver resulting in a reduction of apoB100-containing VLDL particles and their remnants in the circulation and increase clearance of chylomicrons from the circulation. An increase in the EPA to arachidonic acid ratio generates anti-inflammatory mediators such as resolvins and they may have beneficial effects on endothelial dysfunction, and inflammation seen in the arterial wall. In the REDUCE-IT trial, there was a drop in the CRP levels with EPA, however, there was no interaction between baseline CRP and relative risk reduction, which could be expected if it was a strong anti-inflammatory action that drove the benefit. Therefore, other mechanisms responsible for the salutary CV benefits of purified EPA need to be explored. Omega-3 fatty acids are associated with increased bleeding times and reduced thrombogenic potential. Further, EPA stabilizes cholesterol within cell membranes, in a way that DHA does not because of their different physical structures
In the PROMINENT trial, the treatment with fenofibrate, a selective peroxisome proliferator– activated receptor α modulator was studied in 10,497 patients with diabetes with triglycerides levels 200-499 mg/dL and HDL-C <40 mg/dL. Pemafibrate significantly reduced triglycerides by −26.2%, very low-density lipoprotein (VLDL) cholesterol by −25.8%, remnant cholesterol by −25.6%, and apolipoprotein C-III by −27.6%. Despite this, there was no reduction in the primary endpoint with pemafibrate compared with placebo at a mean follow-up of 3.4 years likely because apolipoprotein B levels did not decrease but rather increased by 4.8% in the pemafibrate group.22
Non-high-density lipoprotein cholesterol (non-HDL-C)
Non-high-density lipoprotein cholesterol (non-HDL-C) represents the total cholesterol carried by apoB-containing lipoprotein particles. It is calculated from the standard lipid profile as nonHDL-C =total cholesterol −HDL-C. Since non-HDL-C measures all the apo B-containing lipoproteins, it also correlates with the circulating levels of apo B. Although, non-HDL-C and apo B correlate significantly, yet are only moderately concordant because the cholesterol content per apo B particle is variable. Non-HDL-C gives an estimate of total atherogenic cholesterol mass, whereas apo B is a better predictor of total atherogenic lipoprotein particles. Nevertheless, the ability of non-HDL-C compared with apo B to predict ASCVD events continues to be a point of ongoing discussion.23 Non-HDL-C measurement is more practical due to ease of calculation with no added cost. A meta-analysis of 25 trials including 1,31,134 participants on lipid-lowering therapy inferred that non-HDL-C outperforms apo B for the prediction of CVD.24
Apolipoprotein B (Apo B)
Each apo B-containing particle has a single apo B molecule, thus the levels of apo B in plasma are a measure of the number of apo B-containing lipoprotein particles in plasma. The standardized assays for apo B are available, while some measure only apo B 100, others measure both apo B100 and apo B48. Since apo B48 is present in small quantities even in nonfasting samples, both may be acceptable in routine practice. In certain circumstances like subjects with elevated triglycerides, diabetes, obesity, or very low achieved LDL-C levels, the calculated LDL-C level may underestimate both the total concentration of cholesterol carried by LDL and the total concentration of apo B containing lipoproteins, thus underestimating the risk of ASCVD. About 20% of patients may have discordance between measured LDL-C and apo B levels.
Lipid goals to reduce CV risk
LDL-particle numbers, non-HDL-C, and apo B provide a better assessment of on-treatment residual risk than achieved LDL-C levels. Although statins which lower LDL-C also lower nonHDL-C and apoB, the statin therapy reduces LDL-C to a greater extent than LDL particle numbers, non-HDL-C, and apo B. While LDL-C lowering remains the primary focus of therapy, the Lipid Association of India guidelines propose non-HDL-C as a co-primary target (Table 1).14Besides LDL-C goals, the treatment goals for both non-HDL-C and apoB should be achieved especially in patients with diabetes, obesity, metabolic syndrome, and high triglycerides, in whom measurement of LDL-C levels alone tend to underestimate the risk.
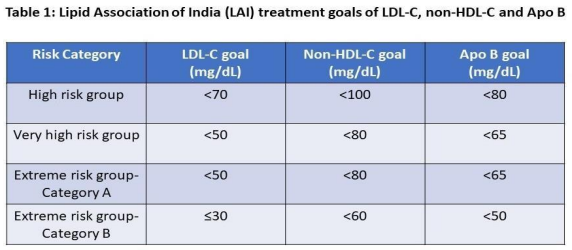
Whether the relative importance of apoB (particle numbers) and non-HDL-C (cholesterol carried by apoB lipoproteins) in atherogenesis differs especially over time and during different stages of plaque development needs further study. Till we have more answers, it is important to achieve LDL-C, non-HDL-C, and apo B goals for optimal reduction of lipid-associated CV risk (Figure 2)
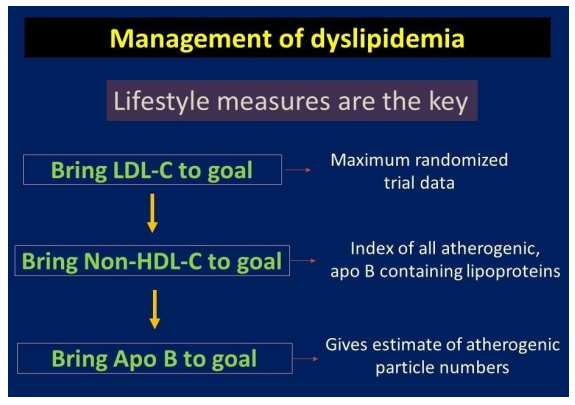
Figure 2. Algorithm for management of dyslipidemia
CONCLUSIONS
The higher the baseline LDL-C levels, the higher the CV risk. Patients with ASCVD and multiple risk factors and comorbidities have a higher risk of future adverse CV events. Hence, they need to be treated aggressively to achieve LDL-C goals. The risk stratification must be done in each patient and the LDL-C goal should be determined. High-intensity statins followed by ezetimibe and bempedoic acid are the way to go in most patients. Lifestyle measures including smoking cessation, alcohol restriction, low-fat diet, regular exercise, weight control in appropriate patients, and adequate control of blood sugar and blood pressure, are important for their desirable effect on lipid profile and reduction of CV risk. Elevated non-fasting plasma triglycerides are a marker of elevated remnant cholesterol. Non-high-density lipoprotein cholesterol (non-HDL-C) represents the total of cholesterol carried by apo B-containing lipoprotein particles. Apo B levels reflect the number of all atherogenic particles. Statin therapy reduces the LDL-C more than apo B by about 15%. On-treatment apo B is a more reliable index of the residual risk. In patients who have achieved LDL goals, non-HDL and apo B goals may be pursued to further reduce the CV risk.
1. Amini M, Zayeri F, Salehi M. Trend analysis of cardiovascular disease mortality, incidence, and mortality-to-incidence ratio: results from global burden of disease study 2017. BMC Public Health 2021;21:401.
2. Krishnan MN. Coronary heart disease and risk factors in India- on the brink of an epidemic? Indian Heart J 2012;64(4):364-7.
3. Huffman MD, Prabhakaran D, Osmond C, et al. Incidence of cardiovascular risk factors in an Indian urban cohort results from the New Delhi birth cohort. J Am Coll Cardiol2011;57:1765-74.
4. The changing patterns of cardiovascular diseases and their risk factors in the states of India: the global burden of disease study 1990–2016. Lancet Glob Health 2018;6:e1339-e1351.
5. Kalra A, Jose AP, Prabhakaran P. The burgeoning cardiovascular disease epidemic in Indians- perspectives on contextual factors and potential solutions. Lancet Reg Health Southeast Asia 2023:12:100156.
6. Mehta V, Iyengar SS, Yusuf J, Mukhopadhyay S, Sattur GB, Puri R. Fighting the atherosclerotic cardiovascular disease epidemic: Declaring war on lipids by Lipid Association of India. J Assoc Physicians India 2020;68(11[Special]):6-7.
7. Ardeshna DR, Bob-Manuel T, Nanda A, Sharma A, Skelton WP 4th, Skelton M, Khouzam RN. Asian-Indians: a review of coronary artery disease in this understudied cohort in the United States. Ann Transl Med 2018;6(1):12.
8. Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): casecontrol study. Lancet 2004;364:937-52.
9. IDF Diabetes Atlas. 10th edition, 2021. https://diabetesatlas.org/data/en/country/93/in.html
10. Geldsetzer P, Manne-Goehler J, Theilmann M, et al. Diabetes and hypertension in India: a nationally representative study of 1.3 million adults. JAMA Intern Med 2018;178:363- 72.
11. Joshi SR, Anjana RM, Deepa M, et al. Prevalence of dyslipidemia in urban and rural India: the ICMR–INDIAB Study. PLoS One 2014;9(5):e96808.
12. Lloyd-Jones DM, Morris PB, Ballantyne CM, et al. 2022 ACC Expert Consensus Decision Pathway on the role of nonstatin therapies for LDL-cholesterol lowering in the management of atherosclerotic cardiovascular disease risk: A report of the American College of Cardiology solution set oversight committee. J Am Coll Cardiol 2022;80(14):1366-1418.
13. Mach F, Baigent C, Catapano AL, Koskinas KC, et al; ESC Scientific Document Group. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 2020;41(1):111-188.
14. Puri R, Mehta V, Duell PB, et al. Proposed low-density lipoprotein cholesterol goals for secondary prevention and familial hypercholesterolemia in India with focus on PCSK9 inhibitor monoclonal antibodies: Expert consensus statement from Lipid Association of India. J Clin Lipidol 2020;14(2):e1-e13.
15. Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 20,536 high-risk individuals: a randomized placebo-controlled trial. Lancet 2002;360(9326):7-22.
16. Puri R, Mehta V, Iyengar SS, et al. Triglycerides and atherosclerotic cardiovascular disease. J Assoc Physicians India. 2020 Nov;68(11[Special]):35-41.
17. Sacks FM, Tonkin AM, Shepherd J, et al. Effect of pravastatin on coronary disease events in subgroups defined by coronary risk factors: the Prospective Pravastatin Pooling Project. Circulation 2000;102(16):1893-900.
18. Bhatt DL, Steg PG, Miller M, et al. Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N Engl J Med 2019;380:11-22.
19. Budoff MJ, Bhatt DL, Kinninger A, et al. Effect of icosapent ethyl on the progression of coronary atherosclerosis in patients with elevated triglycerides on statin therapy: final results of the EVAPORATE trial. Eur Heart J 2020;41(40):3925-32.
20. Nicholls SJ, Lincoff AM, Garcia M, et al. Effect of high-dose omega-3 fatty acids vs corn oil on major adverse cardiovascular events in patients at high cardiovascular risk: The STRENGTH randomized clinical trial. JAMA 2020;324(22):2268-80.
21. Oscarsson J, Hurt-Camejo E. Omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid and their mechanisms of action on apolipoprotein B-containing lipoproteins in humans: a review. Lipids Health Dis 2017;16:149.
22. Das Pradhan A, Glynn RJ, Fruchart JC, et al. Triglyceride lowering with fenofibrate to reduce cardiovascular risk. N Engl J Med 2022;387:1923-34.
23. Puri R, Mehta V, Iyengar SS, et al. Non-HDL cholesterol and atherosclerotic cardiovascular disease. J Assoc Physicians India 2020;68(11[Special]):54-58.
24. Robinson JG, Wang S, Jacobson TA. Meta-analysis of comparison of the effectiveness of lowering apolipoprotein B versus low-density lipoprotein cholesterol and non-highdensity lipoprotein cholesterol for cardiovascular risk reduction in randomized trials. Am J Cardiol2012;110:1468-76.